Table of Contents
In a significant shift that could impact patient care, the American Medical Association (AMA) has adopted a new policy urging doctors to deemphasize the use of body mass index (BMI) as a measure of health. With over 40% of Americans classified as obese according to BMI, this policy statement challenges the long-standing assumption that it accurately predicts an individual’s health risks associated with elevated weight.
Limitations of BMI
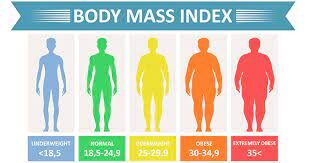
BMI, a metric developed by dividing body weight in kilograms by height in meters squared, gained popularity in the 1990s as the official screening index for obesity following its adoption by the World Health Organization. It is widely implemented in healthcare settings due to its ease of measurement and cost-effectiveness.
However, healthcare professionals have raised concerns about the limitations of BMI. While it shows strong correlations with body fat percentage and the risk of serious health conditions at a population level, it fails to provide precise information about an individual’s body fat composition. Factors such as age, muscle mass, sex, and race can significantly influence body fat percentages, leading to variations in health risks among individuals with the same BMI.
Fat distribution within the body is another crucial aspect that are not accounted for. Research has shown that fat stored around internal organs carries higher health risks compared to fat distributed in other areas. This highlights the importance of considering not just overall body weight but also the distribution of fat when assessing health risks.
How the Scores can Vary
Furthermore, the accuracy of BMI in predicting body fat and health outcomes can vary based on factors such as race, sex, age, and physical fitness level. Different populations may exhibit diverse health outcomes even at similar index levels. For example, individuals with metabolically healthy obesity, defined as having a score above 30 without high blood pressure, blood sugar, or cholesterol, have significantly lower health risks associated with their weight.
The Evolving Understanding of BMI and Health Risks
Historically, studies suggested that any BMI above the normal range (18.5-24.9) could shorten life expectancy. However, more recent research indicates that BMI in the overweight (25-29.9) to class 1 obesity (30-34.9) range may not increase the risk of early death. Improved treatment of conditions like high cholesterol and blood pressure may explain the potentially lower risk of mortality in individuals with higher body weight.

Implications for Patient Care
The AMA’s policy statement reflects a growing recognition among healthcare professionals that BMI alone should not be the sole determinant of health status. Instead, a more comprehensive and personalized approach is needed to assess health risks associated with elevated weight. This shift in perspective could lead to changes in clinical practice, prompting healthcare providers to consider additional factors such as body fat distribution, metabolic health, and individual health outcomes when evaluating patients.
The AMA’s call to deemphasize BMI as a measure of health highlights the limitations of this widely used metric. While it has been a convenient tool for assessing obesity on a population level, its inability to account for individual variability and body fat distribution poses challenges in accurately predicting health risks. Moving forward, healthcare professionals are encouraged to adopt a more holistic approach to patient care, considering a range of factors beyond the index to provide personalized and effective obesity management strategies.