42% of Polycystic Ovarian Syndrome patients had normal BMI, although their clinical and hormonal profiles were identical to those of PCOS patients with increased BMI.
Background
Polycystic Ovarian Syndrome is a completed and wide range of endocrine disorders that occur as a result of a synergistic interplay of genetic, higher oxidative stress, epigenetic, and environmental variables, linked to both metabolic and reproductive imbalances, with short and long-term health effects on women. It is the most prevalent cause of anovulatory infertility affecting 4-8% of women of reproductive age. Even after decades of study, PCOS is still an enigmatic disorder.
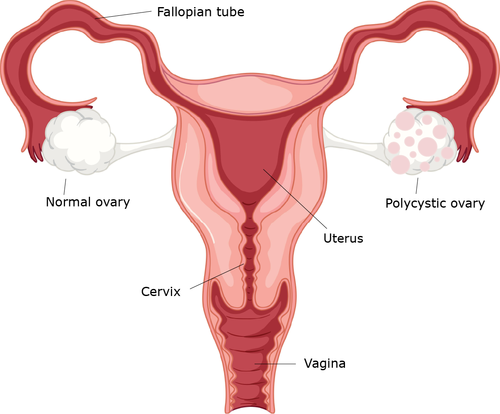
Obese(seen in 50-70% of cases) and lean are the two Polycystic Ovarian Syndrome phenotypes; the latter is a considerably less prevalent form. Common symptoms include polycystic ovarian morphology, irregular menstruation, and hyperandrogenism.
Hyperandrogenism is the overabundance of male sex hormones that leads to hirsutism( excess body hair), androgenic alopecia, and acne on the chest, neck, lower face, and upper aspect of the back (seen in 20-40% cases).
Lean Polycystic Ovarian Syndrome
A lesser but noticeable percentage of females with PCOS have a normal or low BMI (25kg/m2). The majority of these patients do exhibit normal symptoms including acne and irregular menstrual periods. This phenotype of Polycystic Ovarian Syndrome with BMI <25 kg/m² is called Lean PCOS. Diagnostic processes and treatment techniques are more complex in such types, leading to substantial diagnosis delays and exacerbating their complications.
Causes
Another significant finding in people with PCOS is insulin resistance. Increased levels of insulin and glucose have a hormonal impact on the ovaries. They cause the excess production of androgens, which sends a feedback loop to other hormones like estrogen and LH, making them out of sync and less effective in promoting ovulation.
Diagnostic Observations

There is some unanimity that the clinical signs of PCOS in those with lean and obese PCOS are similar.42% of PCOS patients had normal BMI, although their clinical and hormonal profiles were identical to those of PCOS patients with increased BMI. Blood test reports show similarity with high levels of LH, serum insulin, and reduced levels of FSH and estrogen. Lean PCOS can be diagnosed based on these clinical signs and test results. Hence a woman with a normal BMI showing the PCOS-like feature can be a patient of lean PCOS.
Healthy Living with Lean Polycystic Ovarian Syndrome
In the treatment of lean PCOS, nutrition is one of the main modifiable risk factors. To guarantee proper intake of adequate minerals and vitamins, they are advised to eat a better diet with more fruits, vegetables, whole grains, and legumes, including healthy omega-3 fats, especially fatty fish.

Research shows, eating the highest-calorie meal at breakfast and the lowest-calorie meal in the evening helps ease insulin resistance, promote ovulation, and lower testosterone levels in women with lean PCOS. Supplementing with calcium and vitamin D will also be beneficial.
Regular exercise will aid people with lean Polycystic Ovarian Syndrome in maintaining their body mass index. According to the American College of Sports Medicine, HIIT will be extremely beneficial to improve insulin resistance and lower body fat percentage. A one-minute high-intensity interval and a one-minute moderate-intensity interval may be used in HIIT(High-intensity interval training) cardiovascular exercises. Given that the intervals are equal in length, this is referred to as a 1:1 interval.
These lifestyle changes will support frequent ovulation and encourage a healthy hormonal balance. Medicines can be used to address additional particular symptoms. It is important to ensure regular monitoring of cardiovascular disease and other health complications as well.
Although there is a delay in diagnosis for women with lean PCOS, treatment, and therapy results are generally positive. A motivational attitude along with medical treatment can help in maintaining good health for such patients.













