After Alzheimer’s disease, Parkinson’s disease is the most common neurological ailment worldwide. Because the fundamental cause is unknown, a viable cure — or even therapies — remains elusive.
Researchers have recently experimented with a variety of therapies, including hydrogels, personalized brain cell grafts, and just having a better view of the brain. There are still difficulties to overcome.
The majority of Parkinson’s cases are caused by a combination of genetic and environmental risk factors, with the exception of a few unusual cases involving a single gene. However, mitochondrial failure in dopaminergic neurons is a common early symptom of the disease. When a cell is wounded, these tiny factories within it are in charge of producing energy and activating the cell’s self-destruct processes.
Emi Nagoshi, a professor at the University of Geneva (UNIGE) Faculty of Science’s Department of Genetics and Evolution, studied the degeneration of neurons in the fruit fly (drosophila). Nagoshi’s research centered on the Fer2 gene, whose mutation is thought to induce Parkinson’s disease through processes that are still unknown.
Her lab is particularly interested in the Fer2 gene, which encodes a protein that regulates the expression of many other genes and whose mutation may cause Parkinson’s disease through unknown routes.
To find out whether Fer2 plays the same role in mammals, the biologists created mutants of the Fer2homolog in mouse dopaminergic neurons. As in the fly, they observed abnormalities in the mitochondria of these neurons as well as defects in locomotion in aged mice.
“We are currently testing the protective role of the Fer2 homolog in mice and results similar to those observed in flies would allow us to consider a new therapeutic target for Parkinson’s disease patients,” concludes Emi Nagoshi.
The Fer2 gene codes for a protein that controls the expression of other genes. Parkinson’s disease-like symptoms in flies are caused by the lack of the Fer2 gene. As a result, the researchers wanted to explore if having more Fer2 in the cells could help.
Artificial Intelligence and Robotics working towards the study
The New York Stem Cell Foundation’s (NYSCF) enormous bank of patient cells and cutting-edge robotic equipment – The NYSCF Global Stem Cell Array – were used to profile images of millions of cells from 91 Parkinson’s patients and healthy controls.
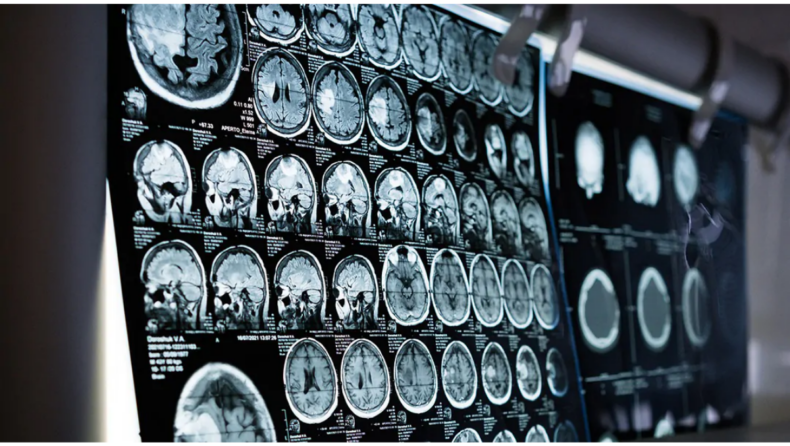
The Array was used to identify and expand fibroblasts from skin punch biopsy samples, label distinct sections of these cells with a technique called Cell Painting, and create hundreds of high-content optical microscopy images.
The generated images were fed into an unbiased, AI-driven image processing pipeline, which identified image attributes unique to sick cells that could be used to differentiate them from healthy controls.

“These artificial intelligence algorithms can figure out what patient cells have in common that might not be visible otherwise,” stated Samuel J. Yang, a Google Research Scientist. “It’s also critical that the algorithms be unbiased — they don’t rely on any existing knowledge or expectations about Parkinson disease, allowing us to find whole new disease markers.”
How will the study be applied?
The team’s discovery of Parkinson disease markers can now be utilised to run pharmacological screens on patient cells to see which medications will reverse these traits. The project also produces the world’s largest Cell Painting dataset (48TB) as a community resource, which is freely available to researchers.
The platform is unique in that it is disease-agnostic, using only easily accessible skin cells from patients. It can also be used on other cell types, such as NYSCF’s induced pluripotent stem cell derivatives, which are used to model a range of disorders.
As a result, the researchers are optimistic that their platform will open up new treatment paths for a variety of disorders where traditional drug discovery has failed.
Published By : VATSAL KOTHA
Edited By : KHUSHI THAKUR