According to UK scientists, participants in a spectacular clinical trial received blood that had been created in a lab(Lab-grown blood). This also has the potential to cure people with sickle cell disease.

A few spoonfuls worth of lab-grown blood is being tried in tiny doses to observe how it reacts in the body. The majority of blood transfusions will always be supported by ordinary donors pulling up their sleeves. However, the ultimate goal is to develop vital but uncommon blood types. For people who frequently need blood transfusions owing to disorders like sickle cell anaemia, they are crucial.
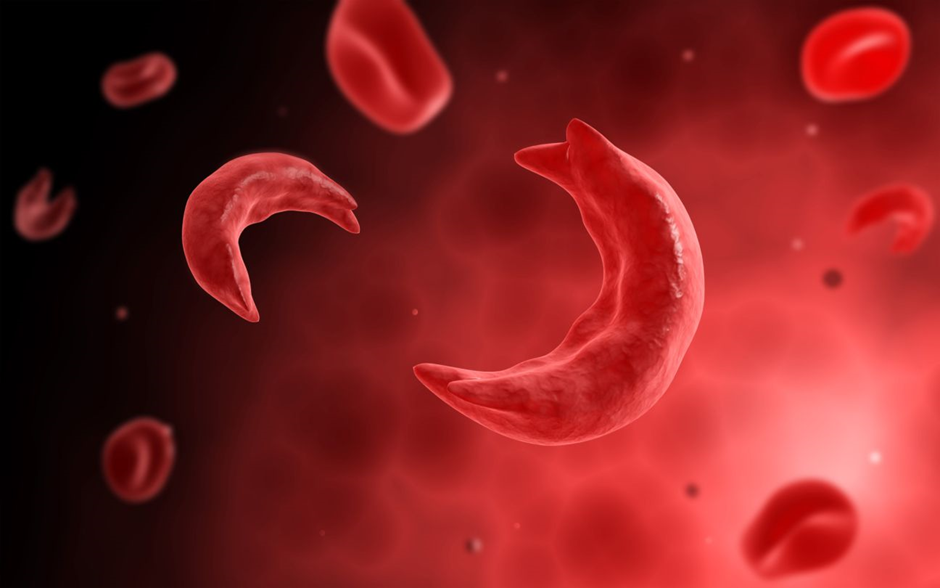
What is sickle cell anaemia?
One of a set of genetic diseases known as sickle cell disease is sickle cell anaemia. The structure of red blood cells, which transport oxygen to every part of the body, is altered. Normally rounded and flexible, red blood cells may flow through blood arteries with ease. Sickle cell anaemia is characterised by red blood cells having crescent-shaped or sickle-shaped haemoglobin. These sickle cells also form a tough, sticky covering that may slow or prevent blood flow. Most people with sickle cell anaemia are incurable. The effects of an illness can be avoided with the use of treatments that lessen discomfort.
If the blood is not a perfect match, the therapy is unsuccessful because the body starts to reject it. Beyond the well-known blood types A, B, AB, and O, this level of tissue matching are present. According to Professor Ashley Toye of the University of Bristol, certain groupings are “very, incredibly rare,” and the number of donors nationwide “may just be 10.”. Only three units of the “Bombay” blood group, which was discovered in India, are now available in the UK.
So, how does the lab-grown blood develop?
The study effort is being carried out by teams from Bristol, Cambridge, London, and NHS Blood and Transplant. The red blood cells, which deliver oxygen from the lungs to the rest of the body, are the main subject of attention.
The process is as follows:
They start by donating a pint of lab-grown blood as is standard (around 470ml)
Magnetic beads are used to collect flexible stem cells with the potential to grow into red blood cells.
These stem cells multiply in large quantities in laboratories before being told to develop into red blood cells.
50 billion red blood cells are produced from an initial pool of roughly 500,000 stem cells during the course of the procedure, which lasts about three weeks.
To get approximately 15 billion red blood cells which are ready for transplant, they are reduced by filtering.

In an interview, Professor Toye said, “The idea in my brain is a room full of machines creating it continuously from a regular blood donation. In the future, we aim to produce as much blood as we can.”
In the experiment, which intends to examine the blood of at least 10 healthy volunteers, the first two participants have already participated. Two donations of 5-10 ml each of normal blood and lab-grown blood will be given to them, at least four months apart.
To track how long the radioactive chemical in the blood remains in the body, scientists have tagged it with a substance that is frequently employed in medical treatments. The lab-grown blood is anticipated to be more powerful than regular blood.
The average lifespan of red blood cells is 120 days before they require replacement. Red blood cells from a regular blood donation are a mixture of young and old, but those from lab-grown blood are 100% brand-new and should survive the whole 120 days. The researchers believe that in the future, this would enable smaller and less frequent contributions. However, there are enormous technological and financial obstacles.
The typical NHS blood donation costs about £130. The price of growing blood will be far higher, however, the researchers won’t disclose it. Another difficulty is that the extracted stem cells ultimately run out of energy, which restricts the potential growth of blood. To create the quantities required for clinical use, further research will be required. ‘Mass-manufactured blood’ is made possible by discovery.
‘This world-leading study sets the foundation for the manufacturing of red blood cells that may safely be used to transfuse individuals with illnesses like sickle cell,’ said Dr Farrukh Shah, he is the medical director of transfusion at NHS Blood and Transplant. “This lab-grown blood approach may provide significant benefits for patients who are challenging to transfuse.”
Read also:https://tdznkwjt9mxt6p1p8657.cleaver.live/blood-pressure-listen-to-heart-beats-keep-healthy/













