Unequal Access to Healthcare in Urban Areas: A Contributing Factor to Multimorbidity Among Low-Income Groups
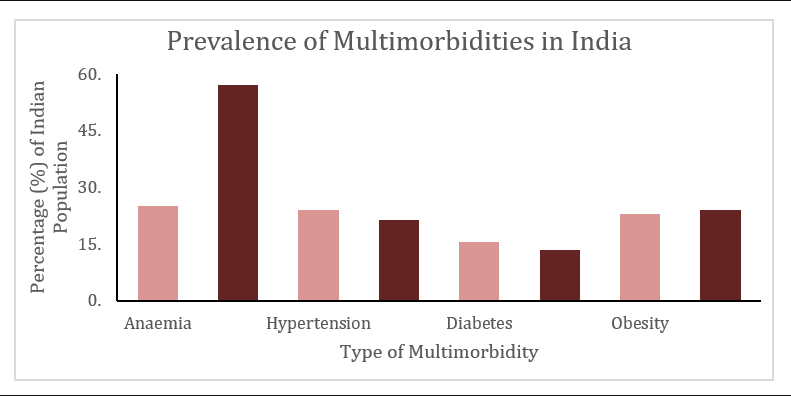
Multimorbidity, characterized by the co-occurrence of two or more chronic conditions, poses a significant health challenge in metropolitan regions of India. The World Health Organization (WHO) defines multimorbidity as a condition that greatly strains an individual’s overall health and well-being. In urban India, common multimorbidities include anemia, asthma, diabetes, hypertension, and obesity. However, low- and middle-income countries, experiencing large-scale rural-urban migration, face even greater burdens due to drastic lifestyle changes upon moving to cities. Among these vulnerable populations, low-income groups are particularly susceptible to multimorbidities, compounded by unequal access to healthcare.
Rapid urbanization and high rates of in-migration contribute to the higher prevalence of multimorbidities in urban areas, particularly in large cities like Visakhapatnam and Hyderabad in the South Indian states of Andhra Pradesh, Tamil Nadu, and Telangana. According to the findings of a research on ‘Patterns of Multimorbidity in India,’ it was observed that in urban settings, the disparity in healthcare accessibility based on gender is particularly prominent. Consequently, women, as the marginalized group, face a higher vulnerability to the onset of multimorbidities.
Income Disparities and Limited Healthcare Access
Income disparities in cities lead to disproportionate access to healthcare, intensifying the impact of multimorbidity. Affordability becomes a significant barrier, especially for low-income groups, who often face high out-of-pocket expenses. Inadequate staffing in healthcare facilities and a lack of awareness regarding their health and risks further impede access to proper healthcare. Additionally, the absence of basic amenities like clean drinking water and sufficient sanitation amplifies the challenges faced by these vulnerable communities.
Research has shown that irrespective of their socioeconomic status, people tend to seek treatment for short-term and minor illnesses while neglecting chronic, long-term diseases, like diabetes, hypertension, and obesity . However, even among those who seek treatment for chronic conditions such as diabetes and hypertension, known to be major comorbidities, inequity persists due to the prolonged duration and higher cost of treatment. The “inverse care law” further compounds this issue, as extensive diagnostic and laboratory testing required for chronic comorbidity treatment escalates costs, limiting access for low-income groups and placing increased stress on physicians.
The COVID-19 Pandemic, Climate Events and Health Implications for Low-Income Groups
The significance of addressing multimorbidity became evident during the COVID-19 pandemic, as individuals with comorbidities faced heightened vulnerability to the virus. Hospitals’ data revealed a higher prevalence of COVID-19 patients with multimorbidities in cities compared to rural areas.
Cities worldwide are witnessing an increase in extreme climate events, such as the urban heat island effect and flash floods. The Urban Heat Island Effect, caused by high-density concrete and infrastructure that absorbs rather than emits heat, leads to elevated temperatures and subsequent health risks. Low-income groups are particularly vulnerable to the negative impacts of extreme climatic events like flooding, droughts, and cyclones due to their substandard living conditions. These events contribute to food and water shortages, food insecurity, malnutrition, and the spread of water- and vector-borne diseases.

Addressing Disparities to Mitigate Multimorbidities
It is crucial to recognize the strong correlation between living in urban areas, socioeconomic status, and access to healthcare. Rapid urbanization and rural-urban migration in India have resulted in significant disparities in healthcare access between high-income and low-income groups.
In conclusion, low-income groups in urban areas face a higher susceptibility to multimorbidities due to unequal access to healthcare. This issue is compounded by income disparities, limited awareness, inadequate basic amenities, and the impact of extreme climate events. Tackling these challenges is essential to promote equitable healthcare access and mitigate the burden of multimorbidities on vulnerable populations.













