INTRODUCTION TO ZIKV
The arthropod-borne Zika virus (ZIKV) belongs to the Flaviviridae family of RNA viruses, which also includes the dengue virus (DENV), the West Nile virus, and the Japanese encephalitis virus.
The necessity for ZIKV-specific vaccinations and antiviral medications has been made clear by the Zika virus’s (ZIKV) emergence as a worldwide health issue. Dendritic cells (DC), which are essential for triggering innate and adaptive antiviral responses, are infected by ZIKV; however, it is unknown how DC function is interfered with in order to cause ZIKV infection.

A genomic profiling technique that permits discrete comparison of primary human DCs infected with ZIKV to nearby DCs that are uninfected, in order to improve the sensitivity and specificity of ZIKV-modulated pathway detection. The findings demonstrate that ZIKV infection particularly boosts the expression of genes with functional enrichment for lipid metabolism.
Sterol regulatory element-binding protein (SREBP) transcription factors are recruited to lipid gene promoters more frequently as a result of ZIKV infection, but SREBP2 is pharmacologically inhibited or genetically silenced to prevent ZIKV infection of DCs. Thus, our data point to SREBP2-activated transcription as an infection-promoting pathway for ZIKV that can be therapeutically targeted.
NEW STUDY

According to LA JOLLA—The Zika virus has a cunning plan. Once a virus has entered the body, it tends to head straight for dendritic cells, which are necessary for an efficient immune response.According to LJI Professor Sujan Shresta, Ph.D., a member of the LJI Center for Infectious Disease and Vaccine Research, dendritic cells are crucial cells of the innate immune system. “How is this virus so cunning that it can infect cells that ordinarily resist infections?”

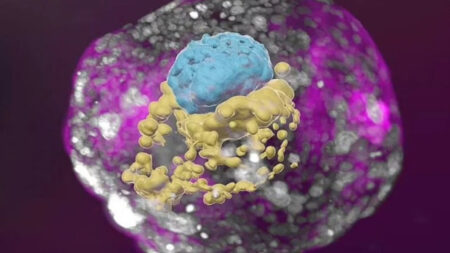
Currently, it has been discovered by Shresta and associates from LJI and the University of California, San Diego, that the Zika virus actually drives dendritic cells to cease functioning as immune cells. The LJI team demonstrated that Zika virus causes dendritic cells to produce lipid molecules instead, which the virus uses to create copies of itself.
ZIKA VIRUS: Here Dendritic cells are aiding a virus in every way possible, claims Shresta.
In order to cure or prevent infection in the future, it is imperative to comprehend how viruses interact with human cells, according to UC San Diego Professor Aaron Carlin, M.D., Ph.D., a former research assistant in the Shresta Lab and co-leader of the new study.
The scientists discovered that the Zika virus affects the genes in dendritic cells that regulate lipid metabolism. A cellular protein called SREBP is summoned by the virus, which causes lipid, or fat molecule, production to ramp up. These lipids served as the building blocks for the assembly of new Zika virus copies, copies designed to circulate throughout the body and propagate infection.
The group then looked into whether Zika converts different cells into lipid factories. The researchers demonstrated that Zika does not affect the lipid metabolism genes in neural precursor cells, despite the virus’s known ability to target them. Shresta was taken aback by the fact that only dendritic cells had undergone these alterations, as well as the fact that Zika and not dengue had affected lipid production.
The viruses are insane, claims Shresta. It depends greatly on the virus and the cell type in question how these viruses alter host cell responses.
The creation of antivirals that stop Zika from using the genes involved in lipid metabolism is the next step. The most recent research suggests that therapeutic SREBP suppression may have promise.