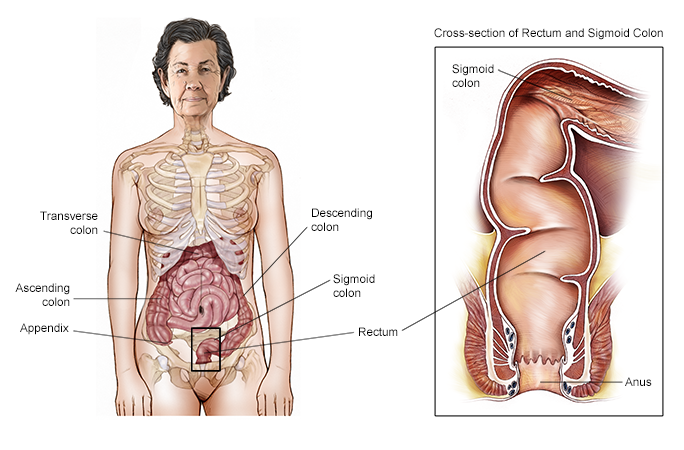
Raising awareness and offering education on screening recommendations, methods, and benefits within the framework of the Affordable Care Act (ACA) are crucial for enhancing outcomes among individuals at risk of colorectal cancer (CRC). Research presented at the American Academy of Physician Associates (AAPA) national conference in Nashville, Tennessee, from May 20 to 24, 2024, suggests that customizing interventions to specific cultures is recommended to improve screening rates and facilitate early detection in racial and ethnic minority groups.
The authors observed a notable lack of awareness among older adults from specific racial and ethnic backgrounds regarding the benefits provided by the Affordable Care Act (ACA) and the recommended age to begin colorectal cancer (CRC) screening. They emphasized that proper screening can effectively reduce the risk of developing CRC.
In order to examine screening rates, researchers conducted a cross-sectional study focused on residents in South Los Angeles County, predominantly consisting of Latino/a/x and Black/African American individuals. The study aimed to explore the knowledge, attitudes, beliefs, and screening practices of adults living in a community setting. Participants included individuals between the ages of 45 and 75 who had no previous history of colon cancer or terminal illness.
Out of the 120 adults enrolled in the study, 57% were female and 43% were male. The researchers observed that 52% of the participants identified as Latino/a/x, while 44% identified as Black/African American. It was noted that 46% of individuals had an annual household income of less than $10,000, although 13% reported having health insurance. Regarding educational attainment, 31% of participants confirmed completing high school and obtaining a diploma.
To collect data, participants were asked to complete a comprehensive survey consisting of 66 questions. The survey covered various topics, including knowledge, attitudes, and beliefs related to colorectal cancer, screening practices, and medical insurance. The survey results revealed that individuals identifying as Black or African American were more likely to be unfamiliar with the benefits offered by the Affordable Care Act (ACA). Additionally, these participants may have a lower perception of their own risk for colorectal cancer compared to the Latino/a/x population.
Members of the Latino/a/x community face obstacles in accessing CRC screening due to fear and a limited understanding of the testing process. Around 30% of the participants expressed the belief that undergoing CRC screening increases their avoidable risk.
In the study, being up to date with CRC screening was defined as having had a colonoscopy within the past 10 years or a home test within the last 3 years. Despite participants acknowledging the benefits of screening, approximately one-third of them were not up to date with the recommended screenings. Furthermore, 40% of those who were not up to date had no intentions of undergoing screening within the following year.
The findings from this study offer valuable insights that can inform the development of targeted strategies to improve the health outcomes of communities at risk. Understanding individuals’ knowledge, beliefs, and screening behaviors related to early cancer detection can have a significant impact on their quality of life and lifespan, particularly as cancer outcomes and health disparities are influenced by factors such as race, ethnicity, and socioeconomic status.
The researchers acknowledged certain limitations of the study, such as the relatively small sample size of only 120 participants from a single site and potential bias resulting from the use of snowball sampling.
According to the researchers, physician associates (PAs) are in an ideal position to address colorectal cancer (CRC) health disparities by enhancing patient knowledge and addressing barriers associated with CRC screening in at-risk communities.