Clinically diagnosed Alzheimer’s disease (AD), post-traumatic stress disorder (PTSD), and traumatic brain injury (TBI) are linked to epidemiological research.
Table of Contents
Medical professionals have never before investigated the effects of traumatic brain injury (TBI), post-traumatic stress disorder (PTSD), and genetic risk factors in a sizable cohort.
Earlier researchers find that there is no connection between post-traumatic stress disorder (PTSD) and/or traumatic brain injury (TBI) and elevated levels of biomarkers associated with Alzheimer’s disease (AD) among veterans. Despite the fact that veterans who had TBI, PTSD, or both exhibited worse cognitive states, earlier experts think it is due to other concomitant diseases.
Brain Injury, PTSD, And Alzheimer’s Disease
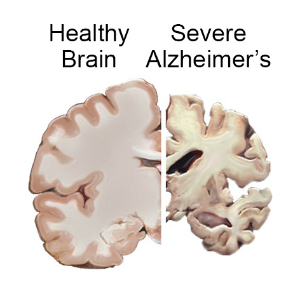
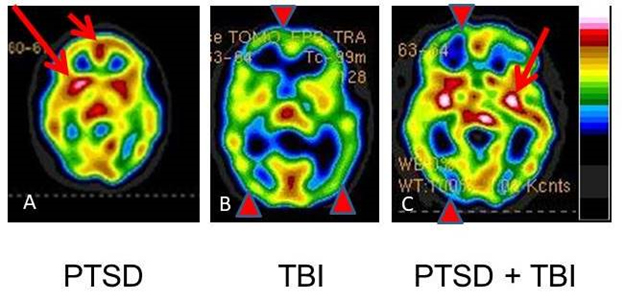
Post-traumatic stress disorder (PTSD) is a mental condition that can develop after being exposed to severe stress. The long-term effects of traumatic brain injury (TBI) include neurological illness and cognitive impairment. A history of moderate-to-severe TBI has been linked to a rough doubling of the risk of dementia. PTSD has also been linked to dementia formation later in life, similar to TBI. PTSD and TBI frequently co-exist.
Researchers found that PTSD, TBI, and the e4 variation of the APOE gene exhibited high links with Alzheimer’s disease and associated dementias in a study of Veterans conducted by the statistician of the National Center for PTSD at the VA Boston Healthcare System, Dr. Mark Logue.
Research Findings
In veterans of European ancestry who acquired the e4 mutation, the study discovered an increase in risk for PTSD and TBI. The effect of PTSD on veterans with African ancestry was unaffected by e4, while the effect and interaction of TBI with E4 were considerably more pronounced. According to other research findings, e4 may amplify the consequences of a brain injury and/or combat-related stress. The study findings are published in Alzheimer’s & Dementia.
“These additive interactions suggest that the incidence of ADRD linked to PTSD and TBI increased with the amount of inherited APOE e4 alleles,” according to research by Logue and colleagues.
One of the world’s biggest databases of health and genetic data, the Million Veteran Program (MVP), provided the researchers with the information they needed to conduct their study.
The percentage of veterans who are at risk for Alzheimer’s and other kinds of dementia is growing, with more than 40% of them being over 75. Logue and his colleagues investigated this further by examining these risk variables combined with the APOE e4 mutation. Large cohort studies have demonstrated that PTSD and TBI increase the incidence of dementia in Veterans. Most people do not inherit the variation, but those who do acquire it from either one (one copy) or both (two copies) of their parents.
From Researchers
According to Logue, a Boston University professor, and military veteran, research has proven that having two copies of the gene e4 significantly increases one’s chances of being diagnosed with Alzheimer’s. He went on to explain that the risk of getting Alzheimer’s increases with age, regardless of APOE genotype, but the discrepancy between those with and without e4 is most prominent between the ages of 65 and 70. He clarified that this doesn’t mean that the risk of Alzheimer’s is reduced after that age, but rather that the risk of both groups is lessened.
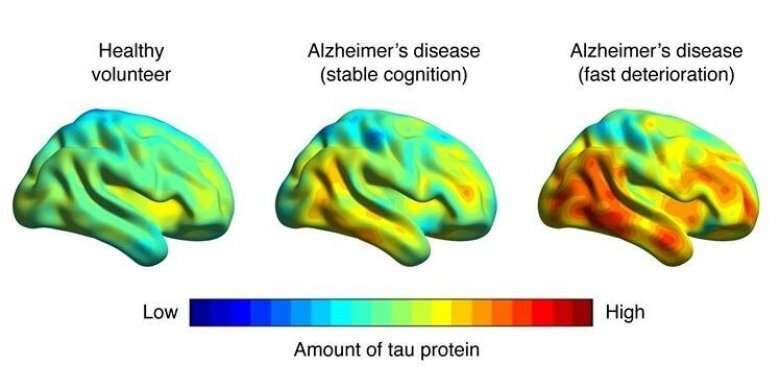
The study revealed that e4 carriers had a higher chance of developing PTSD and suffering a head injury. Using their model, the researchers predicted that the percentage of ADRD would be 6% higher for 80-year-old Veterans of European ancestry who didn’t receive the e4 variation. However, the probability of ADRD for 80-year-old Veterans of European ancestry who inherited two copies of e4 would be 11% greater for those with PTSD than for those without.
Logue was astonished to see such convincing proof of a connection between PTSD and head trauma risk for dementia.
Logue and his team are aiming to use the MVP data to investigate other risk factors related to Veterans and to pursue genome-wide association studies to search for novel dementia and Alzheimer’s risk mutations. It is necessary to take PTSD and TBI history into consideration to make sense of the outcomes of ADRD genetic testing and to correctly carry out ADRD risk assessments.
Even though genetics play a major role in the likelihood of developing Alzheimer’s, it does not give the complete picture. According to Longue, “there is not a single genetic test that can tell if someone will definitely get the disease. The tests can only give a rough idea of the risk of getting it, compared to the average. Our research showed that factoring in other aspects, such as PTSD and head injuries, can help make estimations more accurate. This data is especially relevant for Veterans, and using it will improve the precision of assessing the chance of getting dementia.”













