Table of Contents
Candida auris is labeled as an urgent threat by the Centre of Disease Control and Prevention. It has been observed that it is rapidly spread throughout the world’s health care facilities since it was isolated first in 2009. There have been more than 4000 cases reported since its first case.
It was first seen in an old woman from Tokyo, Japan in 2009, she was suffering from ear infection due to it. Second case was seen in 2011 in South Korea. Since then it has spread to European and Asian countries at a rapid rate. Ultimately it spread to the USA with the first case appearing in 2013.

But why are we so concerned about this fungus and considering it an urgent threat? This is because Candida auris is a fungus resistant to many antifungal drugs. As its case numbers are increasing and it is spreading around the world, it is evolving and undergoing genetic mutation continuously giving rise to new strains resistant to more antifungals.
Since 2016 there has been a continuous rise seen in the number of cases and it even tripled during the phase of increased covid infections. This is owing to the fact that fungal infection occurs in patients with weakened immune system and it was seen consequently that the patients infected with Covid 19 had a very weak immune system either due to infection or due to taking heavy doses of steroid.
The steroids are the mainstay in the treatment of moderate to severe Covid 19 infections. Many experts have observed that they are one of the main reasons for the rapid rise of Candida auris infection in recent years. The uncontrolled rise in blood sugar seen on giving steroids to a patient is one of the main reasons behind it. So, if blood sugar of a patient can be controlled properly by giving drugs or insulin, there is a possibility of controlling the rise of Candida auris infection or many other fungal infections associated with rise in Covid 19 cases.
Candia auris infection: should we worry?
This fungus has many aspects to it and they are all worrying. The rapid spread of this fungus has caused it to become resistant to Echinocandins, which is an antifungal medication recommended for the treatment of Candida auris. CDC has warned that this fungus causes outbreaks in healthcare facilities especially in ICU units where many critical patients are kept.
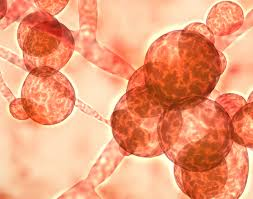
Candida auris invades the bloodstream and can cause infection at any site of the body, with dangerous sites being heart, lungs and brain. The mortality associated with Candida auris infection is quite high with more than 1 patient out of 3 dying if they have this disease.
Scientists are trying to manufacture a vaccine against it but presently it is in the initial stages of development and we don’t have a proper vaccine available for it till date. So, till we have a proper defense developed against it, it is recommended to follow safety precautions if you are admitted in an ICU or taking heavy doses of steroids.
Can we identify Candida auris infection?
It is difficult to identify the infection from symptoms only as it is known to mimic many types of conditions. This is due to the fact that it invades the bloodstream and ultimately causes infection anywhere thus mimicking many types of infection.

Experts recommend to get yourself tested if your symptoms do not get better after taking antibiotics and you are a known case of heavy diabetic, a recent Covid 19 patient or on heavy steroid drugs. As Candida auris is difficult to treat with antifungals due to its widespread resistance, preventing it from infecting you becomes an important key to stay healthy and alive.













