Some of the issues seen in long COVID patients were also experienced by individuals who had a common cold, the flu, or viral pneumonia.
Table of Contents
The largest public health emergency of the 21st century is the COVID-19 pandemic. Patients and society are confronted by the long-term health issues linked to COVID-19, also known as long COVID, in addition to the acute symptoms upon infection. It’s crucial for people to be informed of recent developments and take proactive measures with regard to Long COVID in order to manage it effectively.
Long COVID
SARS-CoV-2, a single-stranded RNA coronavirus that causes severe acute respiratory syndrome, is the source of COVID-19. Even in people who are asymptomatic throughout the acute period, COVID-relevant health concerns may persist for years. This marks the onset of Long COVID.
Physiological consequences and multi-organ dysfunction are possible in this virus infection survivors. Long after patients have recovered from COVID-19 infection, the residual symptoms might have a serious impact on their quality of life.

There are several terms used to describe the subacute and long-term consequences of SARS-CoV-2 infection such as “Long Covid”, “Post COVID-19 condition”, “Long-haul COVID-19, “Post-acute COVID Syndrome”.
Symptoms
Long-term COVID generally starts with fatigue (29%), muscular discomfort, palpitations, cognitive decline (28%), dyspnea (21%), anxiety (27%), chest pain, and arthralgia (18%). Long-term COVID patients in the UK are more likely to have fatigue (51%), dyspnea (35%), arthralgia (25%), and concentration problems (25%). SARS-CoV-2 infection as a respiratory virus causes respiratory system impairment in long COVID.

Cardiovascular problems are another common consequence of chronic COVID patients. A direct channel for SARS-CoV-2 infection is provided by the presence of ACE2 receptors on cardiomyocytes. Myositis and cell death can result from persistent cardiomyocyte inflammatory disease. Additionally, long COVID might impact the central nervous system (CNS). Glial cells are activated by persistent neuroinflammation, which causes neurodegenerative diseases. Blood-brain barrier (BBB) disruption that results from SARS-CoV-2 infiltration will further promote neuro-inflammation in the brain parenchyma.
Long COVID And Other Similar Symptomatic Diseases
According to research, heart palpitations, fatigue, chest discomfort, and shortness of breath were among the issues specific to SARS-CoV-2 although other ailments considered long-COVID symptoms didn’t appear to develop more frequently than after other viral respiratory infections (VRIs). The study findings are published in Open Forum Infectious Diseases.

Electronic health record data from 17,487 people who tested positive for COVID-19 at 122 US healthcare institutions before April 14, 2022, was examined by researchers from the Universities of Missouri and Minnesota. The patients were matched with those who had been diagnosed between March 1, 2020, and April 1, 2021, with the common cold, the flu, or viral pneumonia, as well as with healthy controls.
By anticipating diagnoses that take place 30 to 365 days after infection, COVID-19 was compared with a generic VRI for each study outcome. Diagnoses for which SARS-CoV-2 showed a substantial positive correlation with both the VRI and control groups were thought to be exclusive to COVID-19.
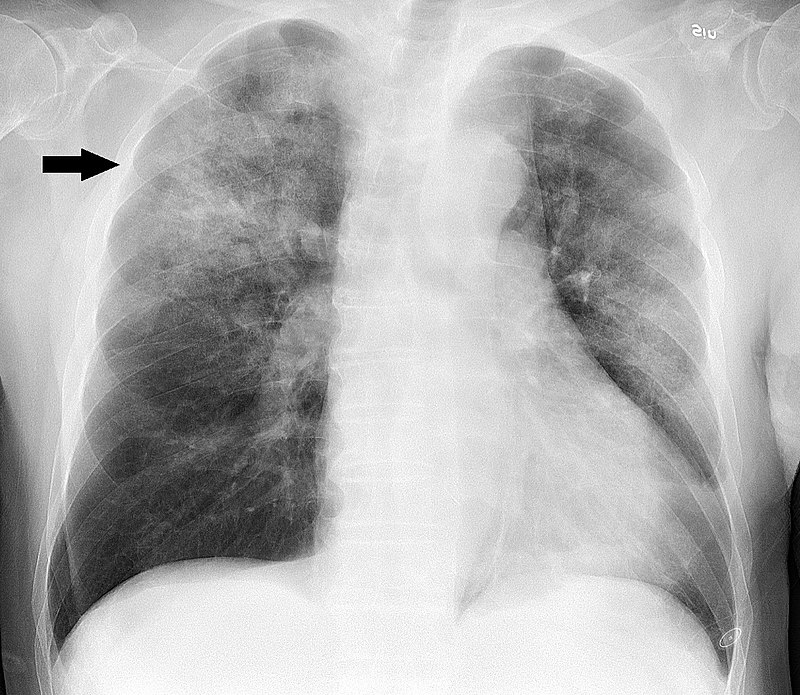
The only lung-related symptoms that were substantially increased in both comparisons of COVID-19 against VRI and COVID-19 versus controls were shortness of breath and chest discomfort. SARS-CoV-2 patients had considerably higher rates of pulmonary embolism (blood clots in the lungs), low oxygen levels, other respiratory failures, the requirement for oxygen, and pneumonia than VRI patients, but not when compared to controls.
Type 1 diabetes, high blood pressure, abnormal cholesterol levels, an abnormally quick heartbeat, and anemia (poor red blood cells) were more prevalent in COVID-19 patients than VRI patients, but not when compared to controls. The average date of the last reported joint pain and fatigue diagnoses was much sooner for COVID-19 patients compared to VRI patients, showing that symptom remission may take place within a year. Researchers said, “The complicated long-term clinical effects of SARS-CoV-2 infection will have a lasting negative influence on patient treatment and quality of life”.